Learn more about common vision conditions with reliable and up-to-date information from the American Optometric Association:
ASTIGMATISM
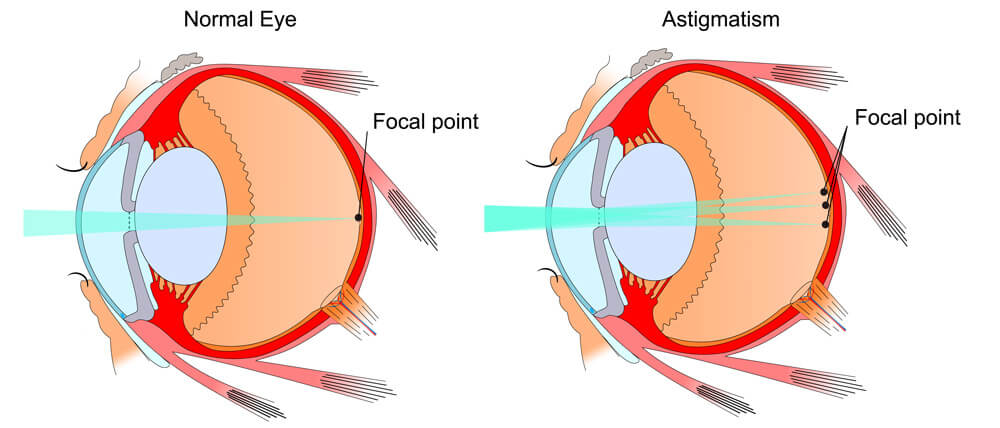
Astigmatism is a common vision condition that causes blurred vision. It occurs when the cornea (the clear front cover of the eye) is irregularly shaped or sometimes because of the curvature of the lens inside the eye.
An irregularly shaped cornea or lens prevents light from focusing properly on the retina, the light-sensitive surface at the back of the eye. As a result, vision becomes blurred at any distance. This can lead to eye discomfort and headaches.
Most people have some degree of astigmatism. Slight astigmatism usually doesn’t affect vision or require treatment.
Astigmatism frequently occurs with other vision conditions like myopia (nearsightedness) and hyperopia (farsightedness). Together these vision conditions are referred to as refractive errors because they affect how the eyes bend or “refract” light.
The specific cause of astigmatism is unknown. It can be hereditary and is usually present from birth. It can decrease or increase over time.
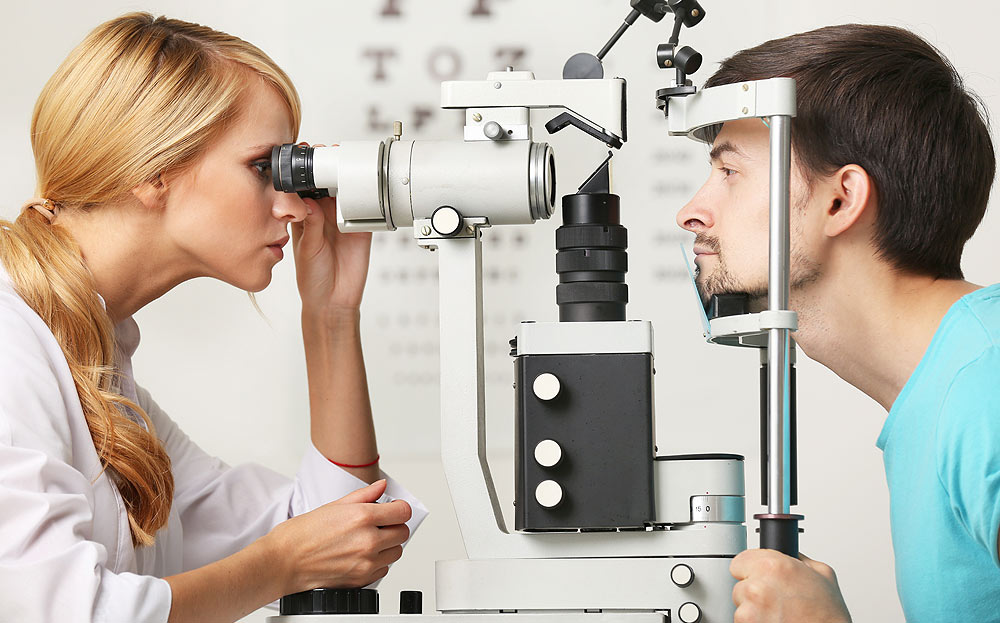
A comprehensive optometric examination will include testing for astigmatism. If necessary, your optometrist can provide eyeglasses or contact lenses that correct the astigmatism by altering the way light enters the eyes.
BLEPHARITIS
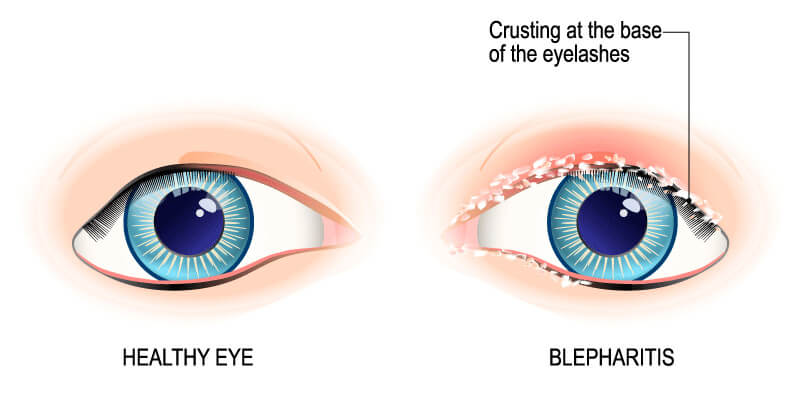
Blepharitis is an inflammation of the eyelids where they become red, irritated and itchy, and dandruff-like scales form on the eyelashes. It is a common eye disorder caused by either bacteria or a skin condition, such as dandruff of the scalp or rosacea. It affects people of all ages. Although uncomfortable, blepharitis is usually not contagious and generally does not cause any permanent damage to eyesight.
BLEPHARITIS IS CLASSIFIED INTO TWO TYPES:
- Anterior blepharitis occurs at the outside front edge of the eyelid where the eyelashes attach.
- Posterior blepharitis affects the inner edge of the eyelid that touches the eyeball.
People with blepharitis may experience a gritty or burning sensation in their eyes, excessive tearing, itching, red and swollen eyelids, dry eyes or crusting of the eyelids. For some people, blepharitis causes only minor irritation and itching. However, it can lead to more severe symptoms, such as blurring of vision, missing or misdirected eyelashes, and inflammation of other eye tissue, particularly the cornea. By touching and rubbing the irritated area, a secondary infection can also result.
In many cases, good hygiene can help control blepharitis. This includes frequently washing the scalp and face, using warm compresses to soak the eyelids and gently washing the eyelids. When a bacterial infection is causing or accompanies blepharitis, antibiotics and other medications may be prescribed.
CONJUNCTIVITIS

Conjunctivitis is an inflammation or swelling of the conjunctiva. The conjunctiva is the thin transparent layer of tissue that lines the inner surface of the eyelid and covers the white part of the eye.
Often called “pink eye,” conjunctivitis is a common eye disease, especially in children. It may affect one or both eyes. Some forms of conjunctivitis are highly contagious and can easily spread in schools and at home. While conjunctivitis is usually a minor eye infection, sometimes it can develop into a more serious problem.
A viral or bacterial infection can cause conjunctivitis. It can also develop due to an allergic reaction to air irritants such as pollen and smoke, chlorine in swimming pools, ingredients in cosmetics, or other products that contact the eyes, such as contact lenses. Sexually transmitted diseases like chlamydia and gonorrhea are less common causes of conjunctivitis.
PEOPLE WITH CONJUNCTIVITIS MAY EXPERIENCE THE FOLLOWING SYMPTOMS:
- A gritty feeling in one or both eyes
- Itching or burning sensation in one or both eyes
- Excessive tearing
- Discharge from one or both eyes
- Swollen eyelids
- Pink discoloration to the whites of one or both eyes
- Increased sensitivity to light
DIABETIC RETINOPATHY
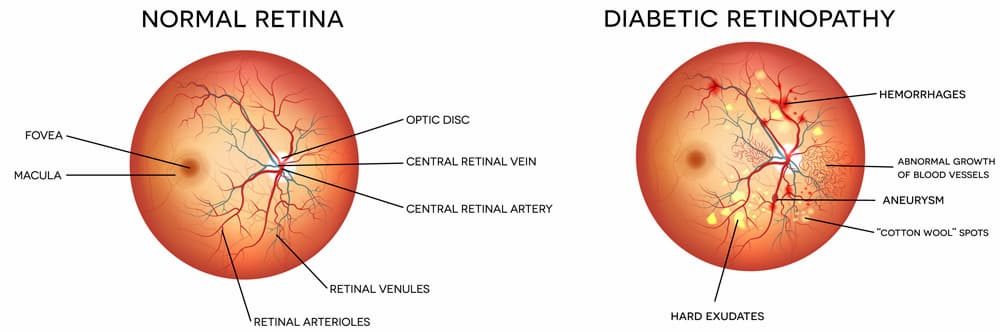
Diabetic retinopathy is a condition that occurs in people who have diabetes. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. Diabetic retinopathy is a serious, sight-threatening complication of diabetes.
Diabetes interferes with the body’s ability to use and store sugar (glucose). The disease is characterized by too much sugar in the blood, which can cause damage throughout the body, including the eyes.
Over time, diabetes damages the blood vessels in the retina. Diabetic retinopathy occurs when these tiny blood vessels leak blood and other fluids. This causes the retinal tissue to swell, resulting in cloudy or blurred vision. The condition usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness.
SYMPTOMS OF DIABETIC RETINOPATHY INCLUDE:
- Seeing spots or floaters
- Blurred vision
- Having a dark or empty spot in the center of your vision
- Difficulty seeing well at night
DRY EYE
Dry eye is a condition in which a person doesn’t have enough quality tears to lubricate and nourish the eye. Tears are necessary for maintaining the health of the front surface of the eye and for providing clear vision. Dry eye is a common and often chronic problem, particularly in older adults.
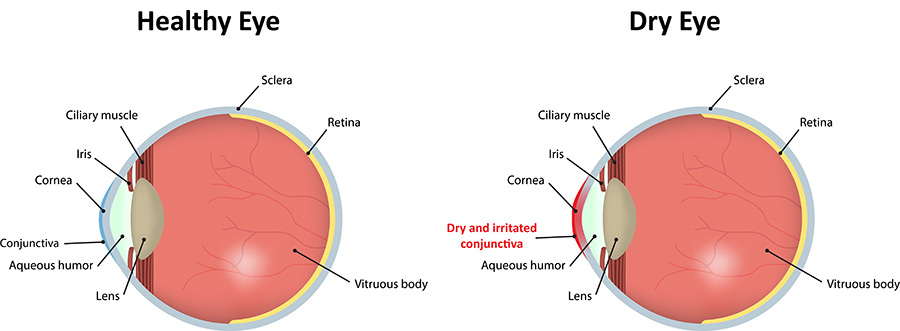
With each blink of the eyelids, tears spread across the front surface of the eye, known as the cornea. Tears provide lubrication, reduce the risk of eye infection, wash away foreign matter in the eye and keep the surface of the eyes smooth and clear. Excess tears in the eyes flow into small drainage ducts in the inner corners of the eyelids, which drain into the back of the nose. Dry eyes can occur when tear production and drainage is not in balance.
People with dry eyes either do not produce enough tears or their tears are of a poor quality:
Inadequate amount of tears. Tears are produced by several glands in and around the eyelids. Tear production tends to diminish with age, with various medical conditions or as a side effect of certain medicines. Environmental conditions, such as wind and dry climates, can also decrease tear volume due to increased tear evaporation. When the normal amount of tear production decreases or tears evaporate too quickly from the eyes, symptoms of dry eye can develop.
Poor quality of tears. Tears are made up of three layers: oil, water and mucus. Each component protects and nourishes the front surface of the eye. A smooth oil layer helps prevent evaporation of the water layer, while the mucin layer spreads the tears evenly over the surface of the eye. If the tears evaporate too quickly or do not spread evenly over the cornea due to deficiencies with any of the three tear layers, dry eye symptoms can develop.
The most common form of dry eyes occurs when the water layer of tears is inadequate. This condition, called keratoconjunctivitis sicca (KCS), is also referred to as dry eye syndrome.
People with dry eyes may experience irritated, gritty, scratchy or burning eyes; a feeling of something in their eyes; excess watering; and blurred vision. Advanced dry eyes may damage the front surface of the eye and impair vision.
Treatments for dry eyes aim to restore or maintain the normal amount of tears in the eye to minimize dryness and related discomfort and to maintain eye health.
GLAUCOMA
Glaucoma is a group of eye disorders that lead to progressive damage to the optic nerve. People with glaucoma can lose nerve tissue, resulting in vision loss.
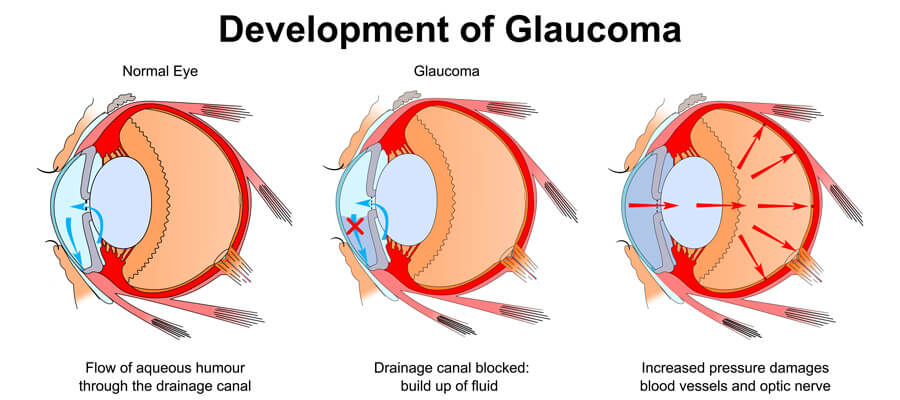
The optic nerve is a bundle of about 1 million individual nerve fibers that transmit the visual signals from the eye to the brain. In the most common form of glaucoma, primary open-angle glaucoma, the fluid pressure inside the eye increases. This increase in pressure may cause progressive damage to the optic nerve and loss of nerve fibers. Vision loss may result. Advanced glaucoma may even cause blindness.
Not everyone with high eye pressure will develop glaucoma, and some people with normal eye pressure will develop glaucoma. When the pressure inside a person’s eye is too high for a particular optic nerve, whatever that pressure measurement may be, glaucoma will develop.
Glaucoma is the second-leading cause of blindness in the U.S. It most often occurs in people over age 40, although an infant (congenital) form of glaucoma exists. People with a family history of glaucoma, African Americans over the age of 40, and Hispanics over the age of 60 have an increased risk of developing glaucoma. Other risk factors include thinner corneas, chronic eye inflammation and taking medications that increase the pressure in the eyes.
The most common form of glaucoma, primary open-angle glaucoma, develops slowly and usually without any symptoms. Many people are not aware they have the condition until they have significant vision loss. Initially, glaucoma affects peripheral or side vision, but it can advance to central vision loss. If left untreated, glaucoma can lead to significant vision loss in both eyes, and may even lead to blindness.
A less common type of glaucoma, acute angle-closure glaucoma, usually occurs abruptly due to a rapid increase of pressure in the eye. Its symptoms may include severe eye pain, nausea, redness in the eye, seeing halos or colored rings around lights and blurred vision. This is an emergency condition in which severe vision loss can occur quickly; see your optometrist immediately.
Glaucoma cannot currently be prevented. But if it is diagnosed and treated early, it can usually be controlled. Medication or surgery can slow or prevent further vision loss.
However, vision already lost to glaucoma cannot be restored. That is why the American Optometric Association recommends an annual dilated eye examination for people at risk for glaucoma. Depending on your specific condition, your doctor may recommend more frequent examinations.
MACULAR DEGENERATION
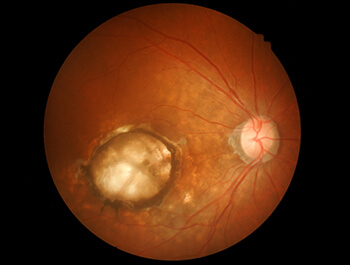
Age-Related Macular Degeneration (AMD) is the leading cause of severe vision loss in adults over age 50. The Centers for Disease Control and Prevention estimate that 1.8 million people have AMD and another 7.3 million are at substantial risk for vision loss from AMD.
Caucasians are at higher risk for developing AMD than other races. Women also develop AMD at an earlier age than men.
This eye disease occurs when there are changes to the macula, a small portion of the retina that is located on the inside back layer of the eye. AMD is a loss of central vision that can occur in two forms: “dry” (atrophic) and “wet” (exudative).
Most people with macular degeneration have the dry form, for which there is no known treatment. The less common wet form may respond to laser procedures and medication injections, if diagnosed and treated early.
SYMPTOMS AND DIAGNOSIS OF AMD
IN ITS EARLY STAGES, THE FOLLOWING SIGNS OF MACULAR DEGENERATION CAN GO UNNOTICED:
- Gradual loss of ability to see objects clearly.
- Shape of objects appears distorted.
- Straight lines look wavy or crooked.
- Loss of clear color vision.
- A dark or empty area in the center of vision.
If you experience any of the above signs or symptoms, contact your doctor of optometry immediately for a comprehensive eye examination. Your optometrist will perform a variety of tests to determine if you have macular degeneration or any other eye health problems.
Central vision that is lost to macular degeneration cannot be restored. However, low-vision devices, such as telescopic and microscopic lenses, can maximize existing vision.
Myopia
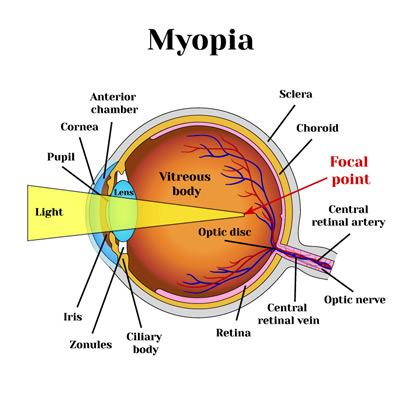
Nearsightedness, or myopia, as it is medically termed, is a vision condition in which people can see close objects clearly, but objects farther away appear blurred. People with myopia can have difficulty clearly seeing a movie or TV screen or the whiteboard in school.
Myopia occurs if the eyeball is too long or the cornea (the clear front cover of the eye) is too curved. As a result, the light entering the eye isn’t focused correctly, and distant objects look blurred.
Myopia affects nearly 30 percent of the U.S. population. While the exact cause of myopia is unknown, there is significant evidence that many people inherit myopia, or at least the tendency to develop it. If one or both parents are nearsighted, there is an increased chance their children will be nearsighted.
Even though the tendency to develop myopia may be inherited, its actual development may be affected by how a person uses his or her eyes. Individuals who spend considerable time reading, working at a computer, or doing other intense close visual work may be more likely to develop myopia.
Generally, myopia first occurs in school-age children. Because the eye continues to grow during childhood, it typically progresses until about age 20. However, myopia may also develop in adults due to visual stress or health conditions such as diabetes.
Myopia may also occur due to environmental factors or other health problems:
Some people may experience blurred distance vision only at night. With “night myopia,” low light makes it difficult for the eyes to focus properly. Or the increased pupil size during dark conditions allows more peripheral, unfocused light rays to enter the eye.
People who do an excessive amount of near-vision work may experience a false or “pseudo” myopia. Their blurred distance vision is caused by overuse of the eyes’ focusing mechanism. After long periods of near work, their eyes are unable to refocus to see clearly in the distance. Clear distance vision usually returns after resting the eyes. However, constant visual stress may lead to a permanent reduction in distance vision over time.
Symptoms of myopia may also be a sign of variations in blood sugar levels in people with diabetes or may be an early indication of a developing cataract.
An optometrist can determine the cause of the vision problems through a comprehensive eye exam.